March 16, 2020
Alcohol use disorder strongly linked to suicide risk, VCU-led study finds
Share this story
Alcohol use disorder is strongly associated with suicide risk, according to a Virginia Commonwealth University-led study published March 12 in the American Journal of Psychiatry.

“[Alcohol use disorder] is a potent risk factor for suicide, with a substantial association persisting after accounting for confounding factors,” concluded the study, conducted by lead author Alexis Edwards, Ph.D., at VCU. “These findings underscore the impact of AUD on suicide risk, even in the context of other mental illness, and implicate the time frame shortly after a medical or criminal AUD registration as critical for efforts to reduce alcohol-related suicide.”
“Alcohol Use Disorder and Risk of Suicide in a Swedish Population-Based Cohort” is part of a series of population studies VCU has conducted with Lund University in Sweden.
This study, completed in 2019 using Swedish population-based registries, had 2.2 million people in its sample. It is one of the largest population-based studies of its kind on alcohol use disorder and suicide in the world, said Edwards, an assistant professor in the Department of Psychiatry at the VCU School of Medicine.
“It’s difficult to translate population-level statistics into individual stories, but one way to think of this is that someone could have come from a great family environment [with] no prominent risk factors — like childhood abuse, or poverty, or a parent with severe mental illness — and if they develop AUD, that alone puts them at a higher risk for suicide,” Edwards said.
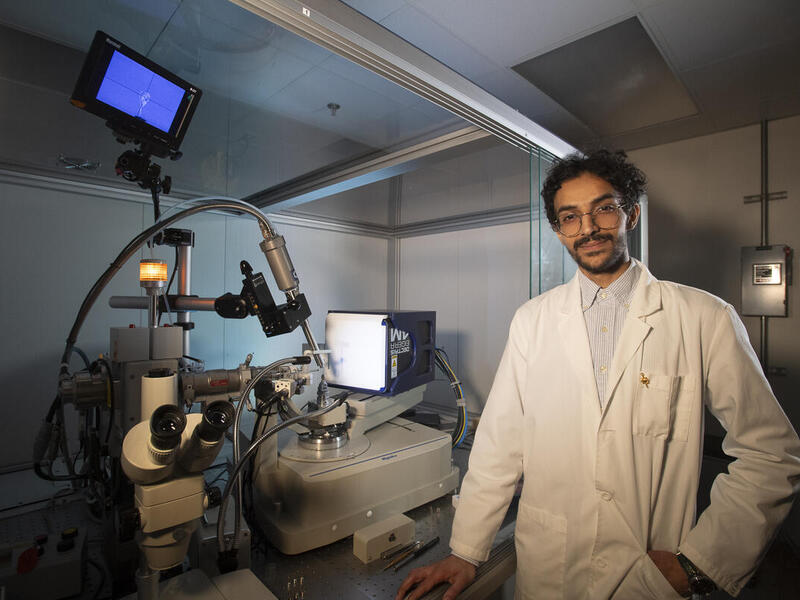
Edwards conducted the research at the Virginia Institute for Psychiatric and Behavioral Genetics at VCU, alongside VCU co-author Kenneth Kendler, M.D., the institute’s director, professor of psychiatry and eminent scholar, and Lund University co-authors Henrik Ohlsson, Ph.D., Jan Sundquist, M.D., Ph.D., and Kristina Sundquist, M.D., Ph.D.
Edwards said taking action is critical to reducing the risk of suicide in individuals with alcohol use disorder.
“The findings suggest that doctors should be especially aware of suicide risk among patients with a history of alcohol use disorder, particularly in the time frame closest to the AUD diagnosis, when risk is highest,” Edwards said. “These patients should be formally assessed for suicide risk.”
It’s difficult to translate population-level statistics into individual stories, but one way to think of this is that someone could have come from a great family environment [with] no prominent risk factors — like childhood abuse, or poverty, or a parent with severe mental illness — and if they develop AUD, that alone puts them at a higher risk for suicide.
The National Institutes of Health’s National Institute on Alcohol Abuse and Alcoholism has awarded Edwards’ team more than $950,000 for the first two years of this four-year study and additional studies related to suicide and substance abuse disorders, including alcohol use disorder.
The NIAAA defines AUD as a chronic disease “characterized by compulsive alcohol use, loss of control over alcohol intake and a negative emotional state when not using.” In 2018, 14.4 million American adults had alcohol use disorder, according to the NIAAA.
“The most striking thing to me was that, even after we control for psychiatric comorbidity — that is, whether someone has depression, or schizophrenia, or an anxiety disorder — there is still a pronounced association between AUD and suicide,” Edwards said. “It’s also really interesting to me that we see evidence for two different mechanisms underlying that association: First, we see evidence that familial factors — both genetic and environmental — contribute to the association, and second, there is evidence consistent with a causal relationship between AUD and suicide death.”
VCU has been among the top 20 institutions for NIAAA funding in 2018 and 2019, as researchers study ways to improve screening for unhealthy alcohol use, curb college drinking practices and increase diversity in the fields of substance abuse and genetics research.
“This study is just one example of how VCU is committed to addressing addiction,” said Peter Buckley, M.D., dean of the VCU School of Medicine and interim senior vice president for VCU Health Sciences and CEO of VCU Health System. “Dr. Edwards’ work contributes to the understanding of the health risks associated with alcohol use disorder.”
Because of the study’s size, Edwards said the findings were consistent in a way that is rare. Having data over decades was crucial to the study, allowing Edwards to examine how the association between alcohol use disorder and risk of suicide shifts over time.
“It was striking to see that the elevated risk persisted for literally decades,” she said.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.