May 10, 2018
VCU graduate students use data, medicine and real-world experience to tackle the opioid epidemic
Share this story
Virginia Commonwealth University graduate students across disciplines are studying how to combat the physical, psychological and societal impacts of opioid abuse.
During the 21st annual Graduate Research Symposium in April, students shared multiple methods for addressing the opioid epidemic, such as improving emergency medical response, and determining the degree to which stress and adversity impact substance abuse. VCU’s Graduate Student Association sponsored the event, part of the eighth annual VCU Research Weeks. This year’s symposium also included a number of topics outside of addiction research.
Research on the abuse of opiates and other substances was highlighted during the symposium as a tie-in with VCU’s 2017-18 common book, “Dreamland: The True Tale of America’s Opiate Epidemic.”
Symposium chair Ellen Stuart-Haëntjens said emphasizing the topic of substance abuse was ideal for VCU.
“At VCU, graduate students from multiple disciplines focus on different aspects of the opioid crisis, ranging from predicting vulnerable communities to improving recovery outcomes and developing both preventative and post-addiction medical treatment,” Stuart-Haëntjens said. “The multitude of departments working on this pressing issue was visible at the symposium when viewing substance-abuse related presentations including the School of Social Work, the School of Medicine and the College of Humanities and Sciences.”
VCU News interviewed several researchers about their work:
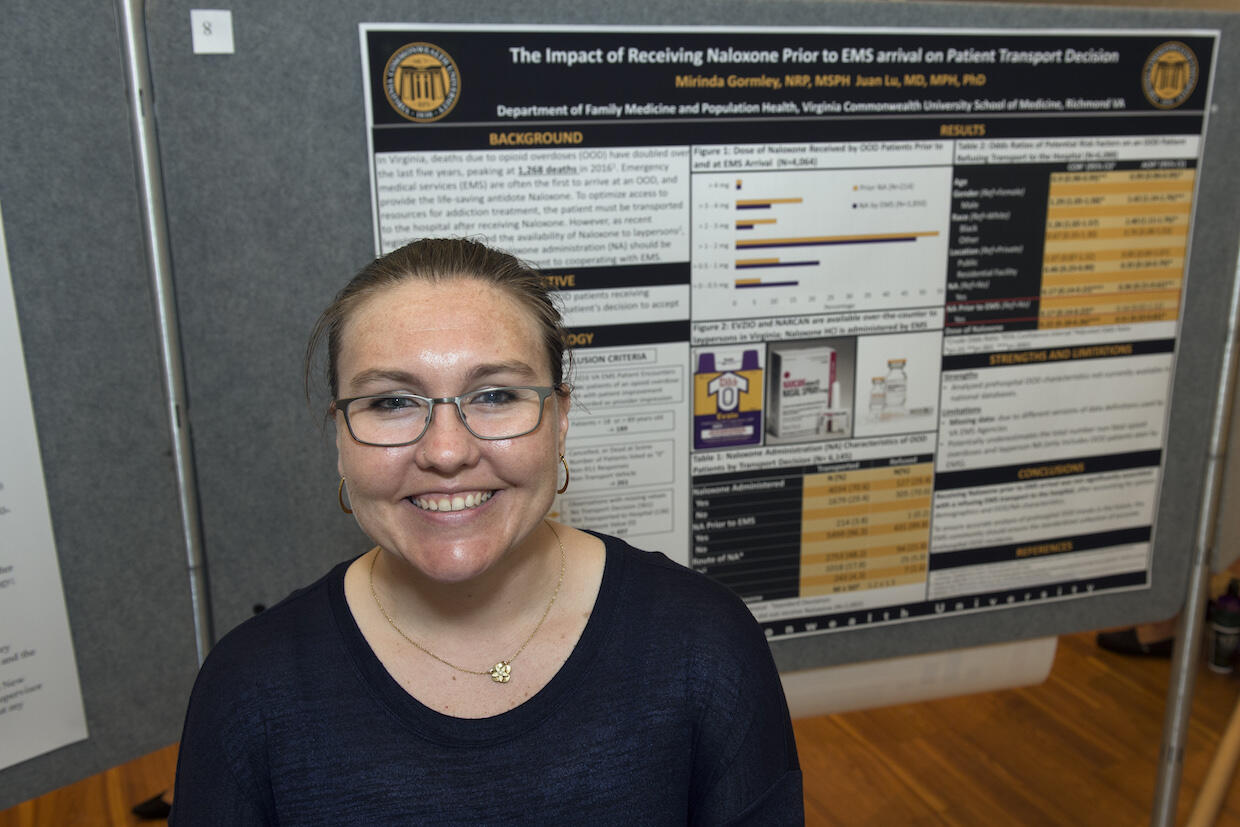
Naloxone and hospitalization
During her 11 years as an emergency medical services provider, Mirinda Gormley estimates that she has responded to dozens of near-fatal overdoses in Richmond. But it’s the four deaths she has responded to that leave the greatest impression.
“I once told a young woman there was nothing else that could be done for her sister,” Gormley said. “This is an epidemic that affects more than drug users; it hurts families.”
Judges recognize work at 21st annual Graduate Research Symposium
Tied for first place: Bhushan Thakkar, College of Health Professions “Relationship between knee valgus asymmetry during running and knee loading during single leg landing in female basketball athletes” Morgan Snell, School of Medicine “Susceptibility to e-cigarette use and risk-taking propensity among smokers and non-smokers” Second place: Athena Cairo, College of Humanities and Sciences “Gray (literature) matters: Selective hypothesis reporting in social psychological research” |
On a Thursday evening last fall, the woman and her boyfriend left their apartment for no more than two hours and returned to find her 20-year-old sister lying on a bare mattress in the living room, staring blankly at the ceiling. Gormley was one of at least 15 firefighters, police officers and EMS responders who crammed into the living room of the tiny apartment to perform resuscitation procedures for nearly a half hour to no avail.
The incident made Gormley, also a Ph.D. student in the Division of Epidemiology in the VCU School of Medicine, determined to do more to prevent drug-related deaths. She used her academic research skills and frontline knowledge of the opioid epidemic to study the potential impact of a recent law intended to make naloxone, a drug that rapidly reverses the effects of opioids on the brain, readily available. Since November 2016, any Virginia resident is legally permitted to request naloxone from a pharmacy without having first visited a health care provider. Gormley analyzed Virginia data to determine if prior administration of naloxone was associated with patients’ refusal of EMS transport to a hospital in cases of opioid overdoses. In all, Gormley reviewed 6,145 cases from 2016, the most recent data available.
In most states, patients are legally permitted to refuse EMS transport to a hospital if they are alert and oriented, even if this happens after receiving treatment from emergency medical services.
“If a patient refuses to go to the hospital, it may be detrimental to them in the long run because it decreases the likelihood they will be able to access resources for opioid addiction treatment,” Gormley said. “I hypothesized that if someone received prior naloxone they would be more likely to refuse EMS transport to the hospital. Due to this increased availability of naloxone, it is possible that the amount of calls we [EMS personnel] receive for opioid overdoses in the future could decrease.”
Gormley will continue researching the association between receiving naloxone prior to the arrival of emergency medical services and patient transport decisions. Results will be submitted to an academic journal this summer.
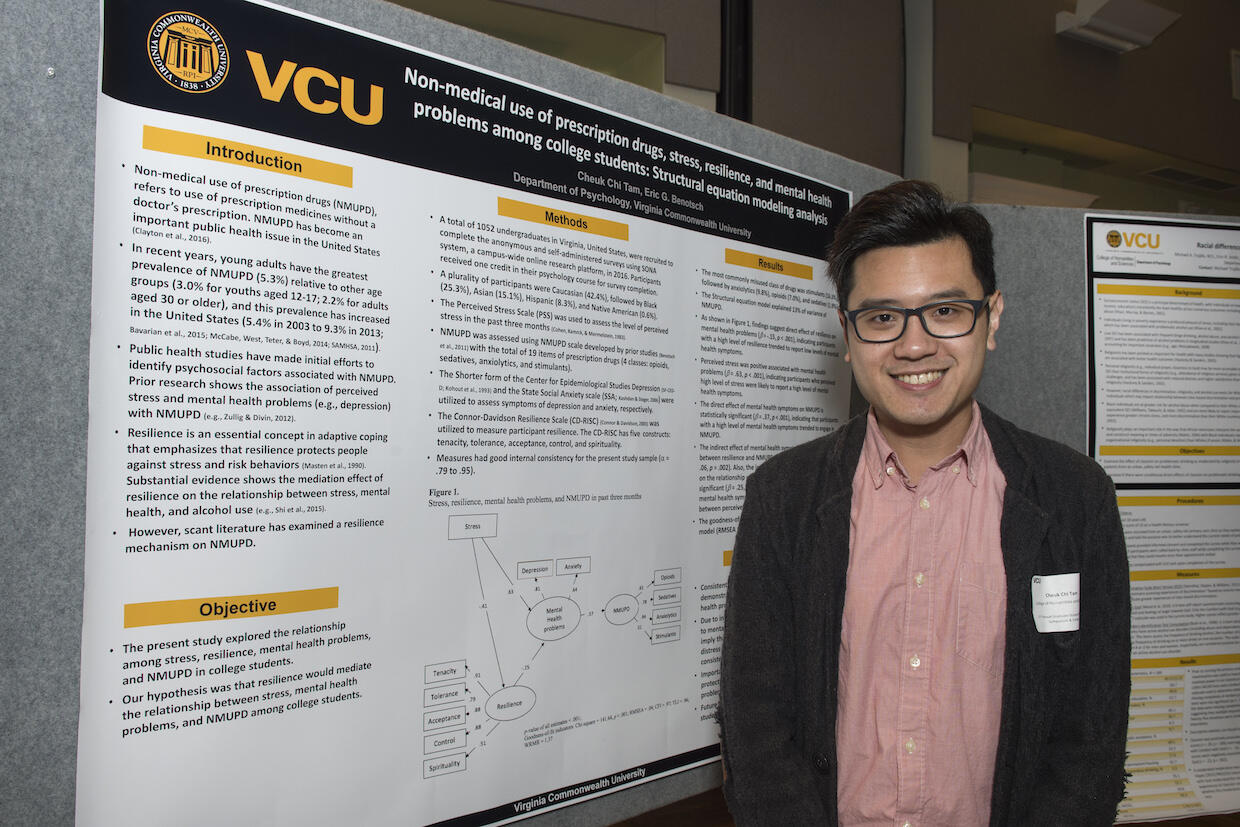
Resilience and prescription drug abuse
Cheuk Chi Tam, a Ph.D. student in the Department of Health Psychology in the College of Humanities and Sciences, studies the connection among resilience, adversity and prescription drug use in college students. Psychologists define resilience as the process by which individuals overcome adversity and stressors.
Abuse of prescription opioids, anti-anxiety medications and ADHD stimulants is highest among young adults, according to the National Institute on Drug Abuse, part of the National Institutes of Health. Studies show that stimulants, often used by college students to increase focus and attention, are the prescription drugs most abused by this age group.
“Resilience, which is a crucial concept in health psychology, has been widely identified as a protective factor against the detrimental effects of stress and adversity on psychosocial and behavioral health,” Tam said. “However, literature on the specific factors of resilience that protect college students against the risk of misusing prescription drugs is scarce.”
Tam said studies on abuse of prescription drugs and other substances found that resilience factors such as self-efficacy, confidence and spirituality might increase coping skills, reducing the likelihood of drug abuse.
Tam added that most resilience studies on young adults and college students within this group have focused on alcohol and cigarette use.
In a study of more than 1,000 American and more than 800 Chinese college students, Tam confirmed the correlation between prescription drug use and resiliency. He also found that Chinese students might differ from American students in patterns of prescription drug abuse. Opiates were the prescription drug most abused by the Chinese students and the third most abused prescription drug class by the American students.
Tam plans to continue studying the factors of resilience most correlated with prescription drug use among Chinese and American college students.
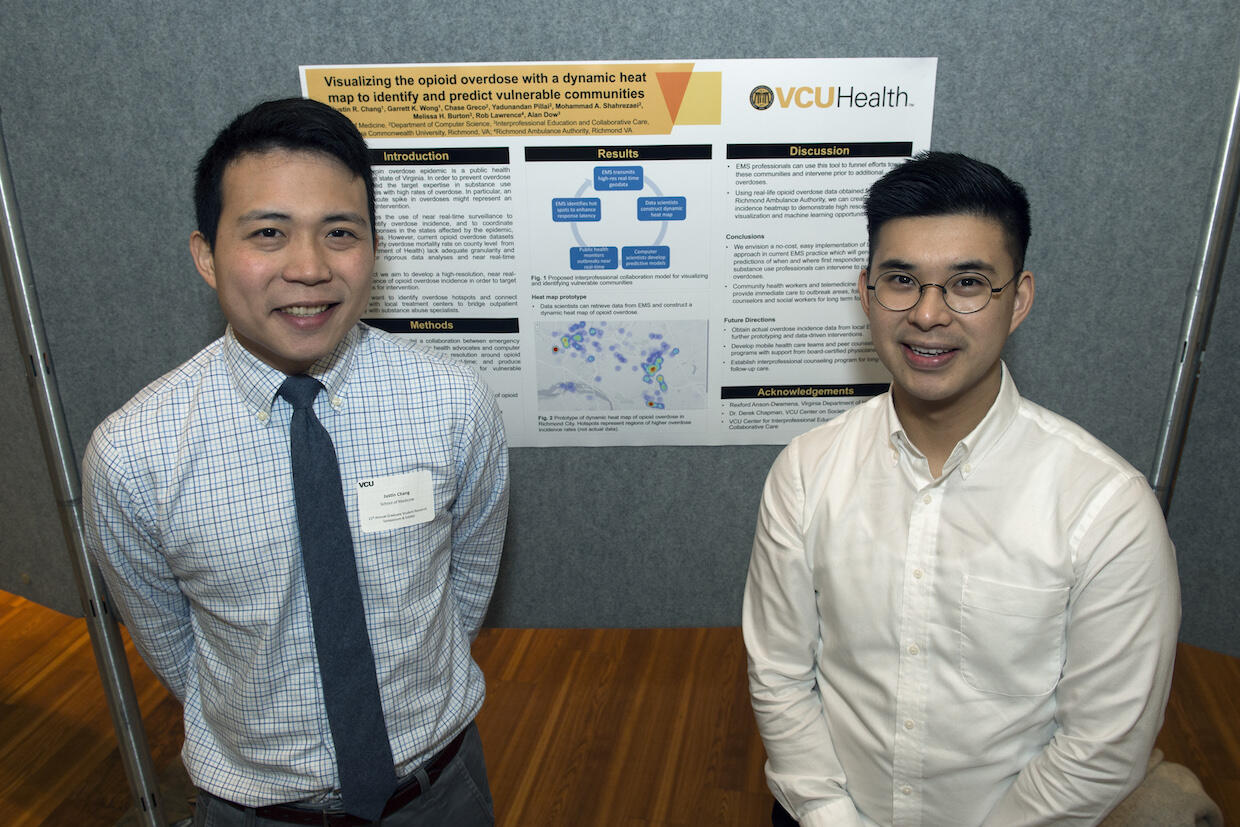
Mapping the problem
Justin Chang, a student in the VCU School of Medicine, is developing a dynamic heat map to help physicians and public health and EMS professionals track opioid overdose hot spots in Richmond. Data on the locations of overdoses provided by local ambulance authorities will be displayed in the final version of the map, which will use changing colors to reflect increased and decreased overdose rates in specific areas over 24 hours.
Chang and his team came up with the idea while participating in the Governor’s Datathon last year. The initiative brings together partners in state government, higher education, private industry and nonprofit organizations to use computer science and data to solve societal challenges.
Former Gov. Terry McAuliffe charged participants with addressing the opioid epidemic. In 2017, 1,227 people in Virginia died of opioid overdose, a 7.8 percent rise from the previous year, according to a Virginia Department of Health report in April. Richmond had the third-highest rate of opioid deaths in the state, at 44.8 per 100,000 people.
Chang and Garrett Wong, also a medical student, advised team members Chase Greco, Yadunandan Pillai and Mohammad Adel Shahrezaei, who study computer science in the VCU College of Engineering, on how to present the hot-spot data to health professionals.
“Red spots on the map represent hot spots, which are areas with higher incidents. It’s a useful tool for EMS and public health professionals and physicians to determine how they can channel resources into these vulnerable areas,” Chang said.
The map will be displayed on a centralized system where health professionals can review the data to inform public health interventions.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.










