Sept. 18, 2012
International Research Team Uncovers How Molecular Parasite Replicates, Spreads Ability to Cause Disease
Share this story
An international team of researchers has uncovered how a molecular parasite responsible for playing a role in antibiotic-resistant disease, such as MRSA, can replicate and spread ability to cause disease, according to a new study published online this week in the Early Edition of the Proceedings of the National Academy of Sciences.
The findings may help researchers identify potential targets to block the spread of infection on the molecular level.
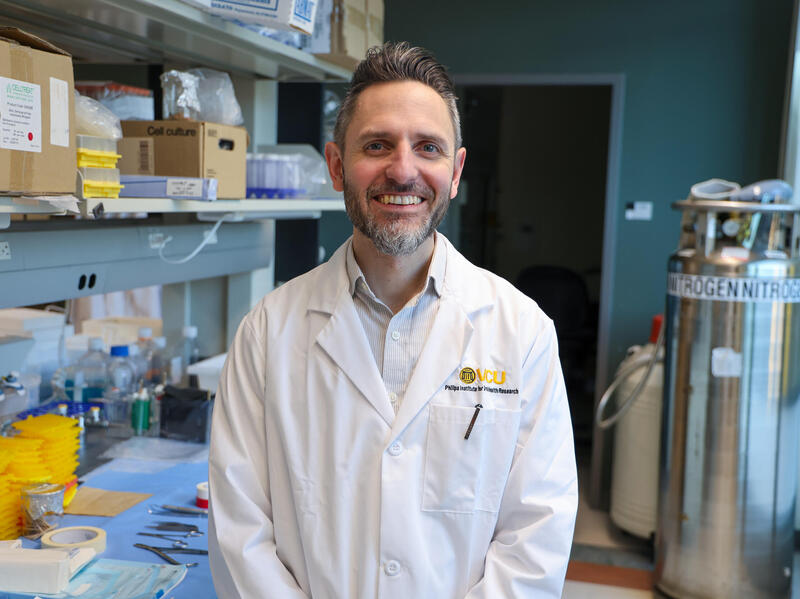
The study was conducted through a longstanding collaboration between researchers from the VCU School of Medicine, the New York University Medical Center and Instituto Valenciano de Investigaciones Agraias (CITA-IVIA) in Spain. The study builds on previous work by the team.
The VCU portion of the study was led by Gail Christie, Ph.D., professor of microbiology and immunology in the VCU School of Medicine, who has spent more than 30 years studying the interactions between bacterial viruses, or phages, and bacterial genomes to gain a better understanding of how disease can spread on the molecular level.
According to Christie, bacterial genomes are constantly changing due to the acquisition of new DNA that can bring in new traits. Genes that grant bacteria the ability to cause disease are often found on acquired pieces of DNA known as pathogenicity islands.
In the pathogen Staphylococcus aureus, which is a major cause of hospital- and community-acquired infections and increasingly resistant to antibiotics, some of the toxin genes that allow this organism to cause disease are carried on a novel, mobile pathogenicity island called a SaPI. SaPI is considered a molecular parasite.
SaPI “hijacks” a bacterial virus to spread among S. aureus bacteria, then directs it to preferentially package the SaPI DNA and carry it to new cells, said Christie. As the SaPI DNA is packaged and passed on, the SaPIs interfere with the growth of their helper phages.
Previous work, by this team with additional collaborators, has focused on one aspect of this interference - the ability of the SaPIs to change the size of the capsid, or head, of the helper phage so that the smaller SaPI genome can be packaged but a complete helper phage genome cannot.
In this new study, the team found a second novel mechanism, which is the specific inhibition of packaging the helper phage DNA into the viral particles. Christie said the team also observed evidence for the existence of a third mechanism.
“Remarkably, different SaPIs use different combinations of these three mechanisms, depending on which particular helper phage they are exploiting,” said Christie.
“Understanding these mechanisms will allow the identification of targets for blocking not only the spread of SaPIs, but of the helper phages themselves - many of which carry additional toxin genes on their own genomes,” said Christie.
According to Christie, this is particularly important because clinical isolates of S. aureus carry both SaPIs and potential helper phages in their genomes, and the replication and spread of these elements can be induced by antibiotic treatment.
The general approach of investigating resistance to SaPI interference by identifying interference-resistant phage mutants was used first in Christie’s lab. Those findings were reported in a research paper published in the journal Nature in 2010.
Christie collaborated with VCU School of Medicine researchers Priyadarshan K. Damle, and Kristin D. Lane, both Ph.D. students in Christie’s lab; Richard P. Novick, M.D., professor in the Departments of Microbiology, Medicine, and Molecular Pathogenesis at New York University Medical Center; Geeta Ram, Ph.D., John Chen, Ph.D., Krishan Kumar, Ph.D., Hope F. Ross, Ph.D., Carles Ubeda, Ph.D., all postdoctoral scholars in the Novick lab; and Jose R. Penades, senior researcher at the Instituto Valenciano de Investigaciones Agraias (CITA-IVIA), in Spain.
This study was supported by a grant from the National Institutes of Health Grants R01AI022159, R21 AI067654 and R56 AI081837.
EDITOR’S NOTE: A copy of the study is available for reporters by contacting the PNAS News Office at 202-334-1310 or PNASnews@nas.edu.
Subscribe to the weekly VCU News email newsletter at http://wp.vcu.edu/vcunews/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Thursday.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.