March 20, 2015
Lifeline: Virginia Poison Center experts are just a phone call away
Share this story
A father walks into his kitchen and discovers his 6-year-old eating table salt by the spoonful. A mom catches her 2-year-old with a mouthful of her medication. A man accidentally drinks bleach out of a coffee cup that was being cleaned. A middle school-aged girl drinks hand sanitizer. These are the types of calls the Virginia Poison Center at Virginia Commonwealth University Medical Center receives on a daily basis, and they barely scratch the surface of the range and complexity of the incidents the center routinely encounters.
In each of these situations, someone has been exposed to a potential poison and needs advice – fast. The Virginia Poison Center’s certified poison specialists are experienced registered nurses and nurse practitioners who have received additional training in the evaluation and treatment of toxic exposures. They are available to provide fast, expert advice; assistance; and supportive care to worried callers 24 hours a day, seven days a week, 365 days a year.
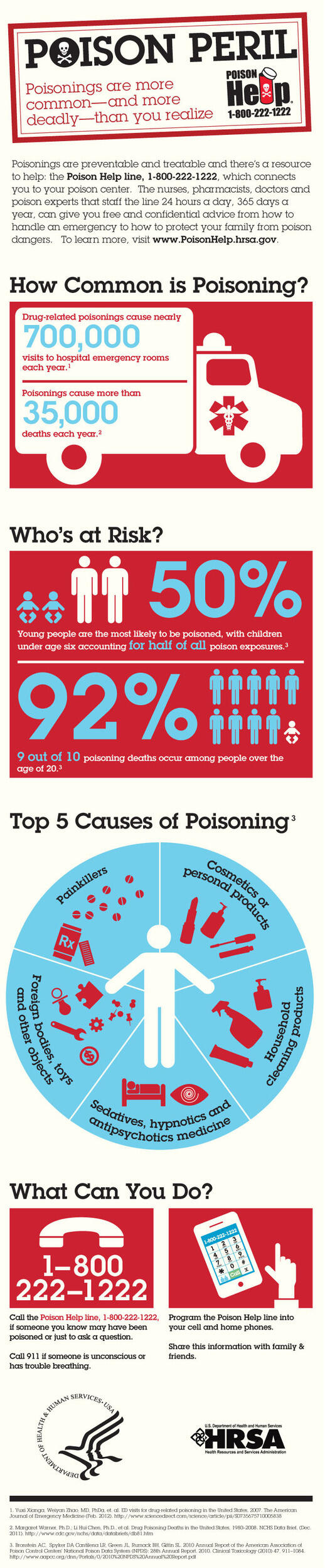
Calling the national Poison Help line at 1-800-222-1222 is the fastest way to obtain accurate information. This toll-free number directs callers located anywhere in the United States to their local poison center based on their area code. The number is not only for emergencies. Specialists and toxicologists are available to give information and answer any questions callers may have.
The Virginia Poison Center received nearly 30,000 calls in 2014, with 25,000 of those calls concerning exposure and another 4,300 calls made for information or advice. The center serves 37 counties and 14 independent cities in southeastern Virginia. This region is home to approximately 3.3 million citizens.
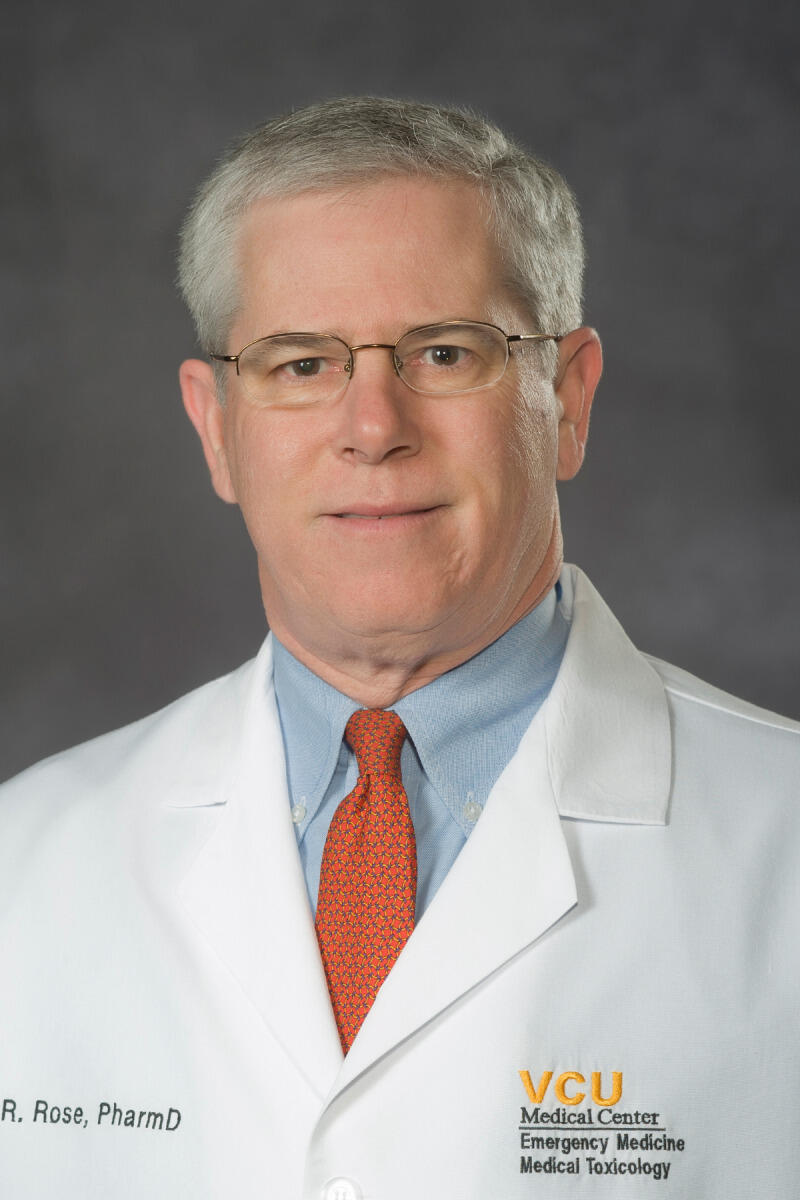
In addition to the calls, “the center helps … several hundred more who get information from health fairs, our website and other sources,” said Rutherfoord Rose, Pharm.D., director of the Virginia Poison Center. “Then we have more than 100 students, residents and other trainees who spend time in the center and use what they learn to help others.”
Examples of poison exposures include overdoses of prescription and over-the-counter medications, bites and stings from animals and insects, ingestion of household chemicals, ingestion of household and wild plants and berries, inhaled fumes or vapors, and chemicals accidentally splashed in the eyes or on the skin. The VPC has seen an uptick in calls over the past two to three years in trending drugs such as synthetic marijuana or “spice,” liquid nicotine and laundry detergent pods.
Another common reason to call the hotline is for assistance with an adverse reaction to a medicine, food or other product that has been used in the correct way, but that has caused a negative health effect.
In addition to a fast response to their initial call, each caller receives individual attention from a specialist until the case is completely resolved, which occurs when the caller no longer presents symptoms or, in serious cases, when the patient is discharged from the hospital. The VPC makes about 35,000 follow-up calls per year.
National Poison Prevention Week
Poisoning is the No. 1 cause of injury death in the United States, with most of these deaths due to drug and medicine misuse and abuse, according to the Centers for Disease Control and Prevention. Since 1962, the president has proclaimed the third week in March as National Poison Prevention Week to raise awareness about the dangers of poisonings and the best ways to prevent them.
This year’s observance focuses on several poison prevention-related themes including “Children Act Fast … So Do Poisons,” “Poison Centers: Saving You Time and Money,” “Poisonings Span a Lifetime,” “Home, Safe Home,” and “Medication Safety.”
Human exposure can occur anywhere, including workplaces, schools, and health care facilities, but in 2013, 93 percent of exposures occurred at a residence, according to the American Association of Poison Control Centers. About 70 percent of the 2.2 million poison exposures reported to poison centers were treated at home, saving millions of dollars in medical expenses. Poison centers save Americans more than $1.8 billion every year in medical costs and lost productivity.
“When studied by health economists several years ago, poison centers were second only to immunizations in saving health care dollars,” said Rose, who is a professor in the Department of Emergency Medicine in the VCU School of Medicine and chair of the Division of Clinical Toxicology. “While poison centers do not make money, they provide a huge return on investment by preventing unnecessary calls to 911 and emergency department visits. Now there is increasing data that poisoned patients in hospitals may do better, and get out sooner with less cost, when a poison center toxicologist is involved in their care.”
‘Dr. Google’
In the past five to six years, calls to poison centers nationwide have decreased 2 to 3 percent. Likely causes are the significant decrease in the birth rate over the same time period and the growing trend of people turning to the Internet as a source for medical information.
“Currently, ‘Googling’ cannot compare to poison centers, who give the correct answer immediately,” Rose explained. “Searching the Internet often gives many answers and even more questions.”
Currently, ‘Googling’ cannot compare to poison centers, who give the correct answer immediately. Searching the Internet often gives many answers and even more questions.
The amount of time it takes to sift through all of the information and myths found on a typical Internet search can be dangerous when dealing with a potential poison exposure.
For example, one enduring myth is the popular advice to drink milk to coat your stomach to prevent poison from being absorbed into the bloodstream. According to the VPC, this is an “old wives’ tale” that dates back to a time when there was little scientific understanding of how chemicals act in the body.
Another common myth is that someone who has been poisoned will have a sudden illness – vomiting, skin color changes or trouble breathing – that inevitably will occur within minutes of the exposure. In fact, poisoning doesn’t always cause an immediate illness. Many chemicals cause unseen, but deadly, damage to internal organs. Calling a poison center is the fastest way to get the best advice for a specific exposure.
Over-the-counter dangers
“People assume just because a drug doesn’t need a prescription then it must not be harmful,” Rose said. “All over-the-counter drugs, with aspirin being a good example, can be very toxic in high doses.”
Most parents store medicine away and out of sight in a medicine cabinet, but do not think of products such as diaper rash remedies, vitamins or eye drops as medicine. Any medicine, including over-the-counter drugs, can be dangerous if taken by the wrong person, in the wrong amount or in the wrong way. For example, diaper rash products can cause lung damage if inhaled and can cause nausea, vomiting or diarrhea if swallowed. Multivitamins can be poisonous if taken in overdose, with the most serious risks coming from iron or calcium supplements. These products need to be stored safely away from children.
Accidental ingestion of over-the-counter redness relief eye drops and nasal decongestant sprays can also cause serious harm to children, the FDA warns. Ingestion of these products can require hospitalization and can cause coma, decreased heart rate, decreased breathing and sedation. Most of these products do not come with child-resistant packaging.
Poison centers around the country see an increase in calls during the summer, especially for over-the-counter poison exposure. Children are out of school on summer vacation and are typically around the house and outside more frequently. Sunscreens and insect repellents are an important part of summer but should be monitored closely around children. Stings, sunburn and poison ivy and oak exposure are also common in both children and adults. Any over-the-counter creams or medicines used to treat these injuries also should be used as directed and monitored around children.
Education and prevention
The VPC strives to make the public aware of how they can prevent serious injury from poisons. The center responds to requests from schools, civic groups, employers, child care centers and state and local agencies, and provides a variety of programs on poison prevention. Every year, the VPC is represented at dozens of community events such as health fairs, where its displays, magnets, stickers and printed materials provide attendees with information on poison safety.
During National Poison Prevention Week, the center partners with local and state groups in a variety of activities to promote the observance each year, such as sending students from the VCU School of Pharmacy to preschool classrooms to teach the dangers of poisons. Attending toxicologists at the center also give lectures to residents, fellows, emergency medicine physicians and nurses and toxicologists.
The observance of this week raises awareness of the dangers of poisonings and how to prevent them. Poison prevention tips to keep in mind are:
· Keep medicines and household products in their original containers and in a different place than food.
· Keep household products and medicines locked up. Put them where children cannot see them or reach them.
· Always read the label and follow any directions.
· Buy products with child-resistant packaging, but remember, nothing is child-proof.
· Keep purses and briefcases out of children’s reach.
· Never call medicine “candy.” Poisons may look like food or drink. Teach children to ask an adult before tasting anything.
· Take medicine in a place where children cannot watch, because children learn by imitating adults.
· Learn about products and drugs that young people use to get “high.” Talk to your teen or preteen about these dangers.
· Keep houseplants out of children’s reach.
· Keep appliances, furnaces, fireplaces and wood-burning stoves in good repair.
· Have a working carbon monoxide alarm in your house.
Individuals are encouraged to keep the Poison Help line number on hand by programming it into a cell phone or posting it somewhere easy to find in the home, such as the refrigerator. It’s good to know that expert help is just a phone call away when the unthinkable happens.
When calling the Poison Help line, callers should be prepared to relay facts to the specialist who answers. Have the product labels nearby and be ready to answer questions such as the size and ingredients in a product or the amount of dosage in a medication.
Other facts the expert will need to know are the age and weight of the patient; existing health conditions; the substance involved and how it contacted the patient (was it swallowed, inhaled, absorbed through the skin or splashed into the eyes); any first aid given; if the patient has vomited; and the location of the patient and how long it will take to get to the closest hospital.
Subscribe for free to the weekly VCU News email newsletter at http://newsletter.news.vcu.edu/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Thursday. VCU students, faculty and staff automatically receive the newsletter.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.