Jan. 6, 2016
Alumnus heads innovative mobile disaster hospital for FEMA
Share this story
When a disaster strikes, the medical community leaps into action. Hospitals brace for an influx of patients, emergency medical teams seek out those who may be injured, and doctors provide care to their community in a time of great need. But what happens when a tornado, earthquake or hurricane destroys a community’s hospital and prevents people from getting the care they need?
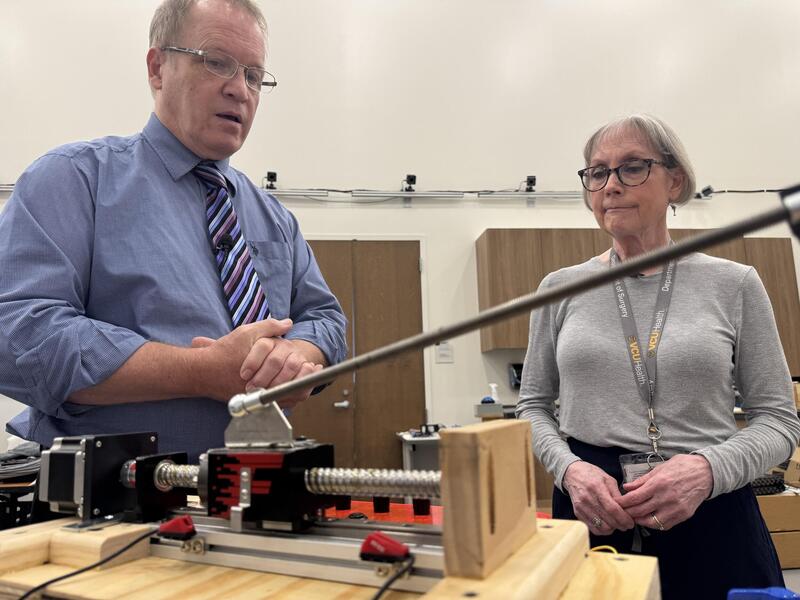
In steps Llewellyn Stringer, M.D., who graduated from the Medical College of Virginia in 1966.
Stringer is the project manager for the National Mobile Disaster Hospital, which is designed to deploy anywhere in the country when disaster strikes. The mobile hospital contains all of the familiar elements of a normal hospital, such as an X-ray unit, blood banks and a pharmacy. This one, however, can be loaded onto tractor-trailers, sent to a disaster area and set up to begin receiving patients within days.
The mobile hospital project was conceived in 2005 after Hurricane Katrina hit New Orleans and left many without access to medical services. The Federal Emergency Management Agency decided it needed to find a way to respond to such disasters, when local hospitals are either damaged or overwhelmed by the number of patients.
Stringer, who served for 10 years as commander of the National Medical Response Team and was the senior medical adviser to FEMA under the Department of Homeland Security, was an obvious choice to lead the project. He retired from FEMA in 2006, but went back to work for the North Carolina Office of Emergency Medical Services. In 2008, FEMA moved the mobile hospital from Maryland to North Carolina, and Stringer took charge again.
The hospital consists of large tents and mobile hard structures. It features a 21-bed emergency department, a 10-bed critical care unit, two operating rooms, full digital X-rays, a small lab, a blood bank, a pharmacy and a central medical supply with enough in storage for 72 hours of operation, a morgue, and an administrative and command control unit.
We can perform just about anything other than open heart surgery.
“We can perform just about anything other than open heart surgery,” Stringer said.
Flexibility is key for Stringer and his team. Their home base in central North Carolina allows them to quickly respond to tornadoes in the Midwest and hurricanes on the East Coast or in the Gulf. “The goal is to deploy within 24 hours of receiving an assignment, bring all units—except the ICU—online within 48 hours after arrival on site and have the ICU operational within 72 hours.”
Collaboration is another central part of the project. The mobile unit is funded by FEMA when deployed, but maintained by NCEMS with funding from U.S. Department of Health and Human Services Assistant Secretary for Preparedness and Response grants. Much of the grunt work of unloading and setting up the hospital is done by volunteers from the N.C. Baptist Men’s Disaster Relief organization, which travels with the hospital when it is deployed.
The volunteers include plumbers, electricians, carpenters and other tradesmen ready to solve any problems that might slow down the hospital’s deployment. Stringer has even partnered with a local North Carolina hospital to make sure he can maintain a stockpile of medical materials that are ready at a moment’s notice.
View in FEMA Multimedia Library
Stringer and his team received their first taste of action last year when the hospital deployed to Louisville, Missouri. The town and its local hospital were badly damaged by a powerful tornado and in need of help. Within days of being deployed, the hospital was able to offer basic services and soon after was able to accept a wide range of patients.
Officials plan to have a temporary hospital open in some capacity in Louisville until 2018 when construction of a new hospital is complete. “Quick response time is obviously an important part of our mission, but maintaining a presence in the affected communities can be equally important,” Stringer said. “One of the major obstacles to New Orleans’ recovery after Katrina was that many of the health care workers had left town. There weren’t hospitals for them to work in.
“In Louisville, we’ve managed to keep 100 of the 140 hospital employees. These people have relationships with their patients and it’s important that they stay in this community to continue providing care.”
The deployment in Louisville also provided an important opportunity to see what worked and what needed to be improved. Nurses told Stringer that showers need to be wheelchair accessible and that they prefer simpler, single-channel IV pumps. Patients requested more private rooms. Doctors asked for improved access to electronic medical records.
Perhaps the biggest problem is one you wouldn’t expect. “Truckers,” Stringer said. “We have all the equipment loaded and ready to go, but it’s hard to find drivers and rigs to haul 23 trailers across the country at the drop of a hat. That hurt our response time.”
Despite the problems he encountered, Stringer said, the first deployment was a success. “I was the senior medical officer for many natural disasters in the country for 10 years, and I can honestly say that the collaboration and sense of community I witnessed on this project was the best I’ve ever seen.”
Subscribe to the weekly VCU News email newsletter at http://newsletter.news.vcu.edu/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Thursday.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.