Sept. 6, 2017
VCU researchers combat opiate addiction
Share this story

Opioids: An American health crisis
Overdose deaths in the United States involving prescription opioids have quadrupled since 1999, according to the Centers for Disease Control and Prevention. Ninety-one Americans die daily from an opioid overdose and more than 1,000 are treated daily in emergency departments for not using prescription opioids as directed. In 2016, Gov. Terry McAuliffe and Virginia Health Commissioner Marissa Levine declared the opioid addiction crisis a public health emergency in Virginia.
At VCU and VCU Health, efforts are underway to combat this public health crisis — through addiction treatment, pain management, health care policy, education and research. This multipart series provides a snapshot of those efforts.
Virginia Commonwealth University researchers are fighting the opioid epidemic by brainstorming more effective clinical approaches, elucidating the biological mechanisms of addiction and developing safer alternatives for pain relief. The university’s opioid-related research spans multiple schools, departments and disciplines, from chemistry to women’s health, and has earned national recognition. VCU’s history of drug abuse research spans decades. For 45 years, the School of Medicine’s Department of Pharmacology and Toxicology has maintained a federal training grant that funds tuition and provides a stipend for graduate students studying drug dependence. The following features some of the innovative work of researchers in the Schools of Medicine and Pharmacy.
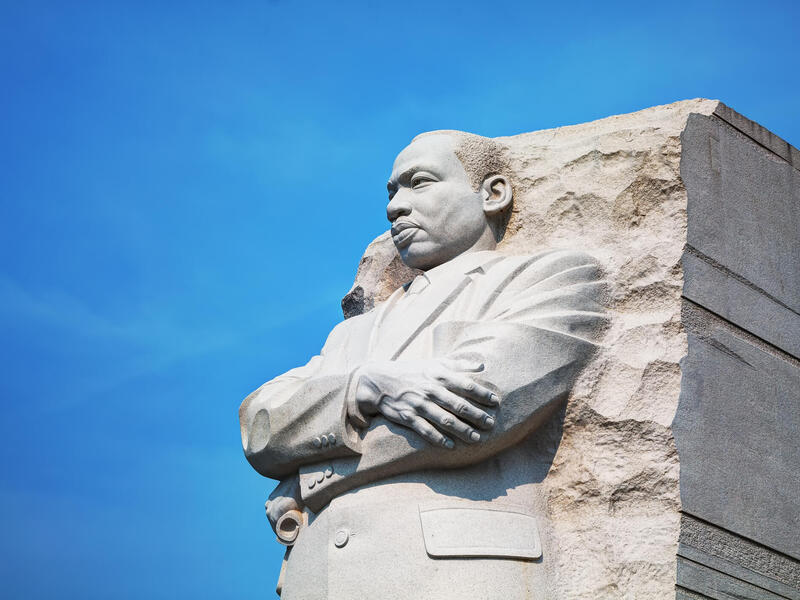
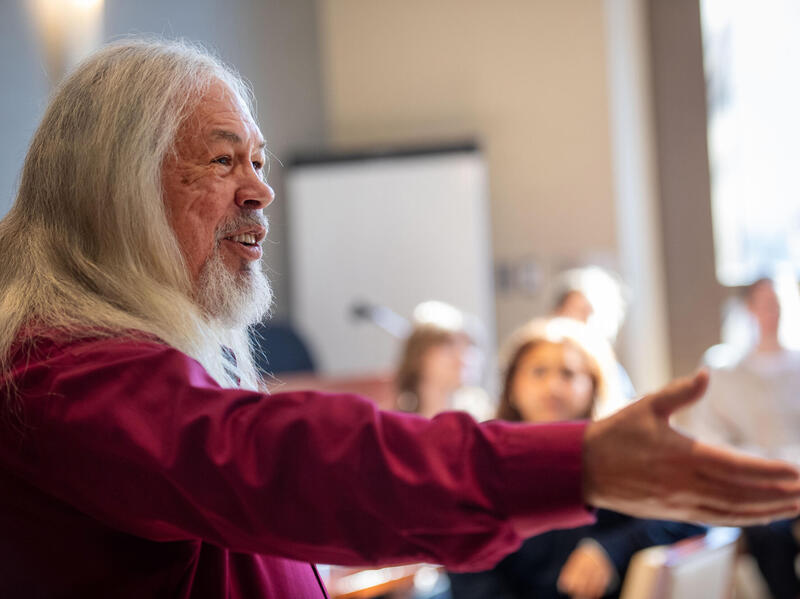
You do research for one reason: to make people healthier. There is no other reason. That is the best way to spend your life – doing things to try to help people.”
-William Dewey, Ph.D., professor and head of the Department of Pharmacology and Toxicology in the School of Medicine

Photo by Burnham Photography.
Yan Zhang, Ph.D., a medicinal chemistry professor at the VCU School of Pharmacy, is working with VCU School of Medicine professors Kurt Hauser, Ph.D., and Dana Selley, Ph.D., to develop therapeutics that would combat neural HIV and opiate addiction. Their work is funded by a $2.72 million grant awarded this summer by the National Institute on Drug Abuse of the National Institutes of Health.

Thirteen years ago, Zhang began developing molecules to target neural reward receptors responsible for opiate addiction. Eventually, he found a link between opiates and neural HIV infection, which is the invasion of the brain by HIV.
In recent years, researchers have observed that a significant number of opiate addicts carry HIV. The disease can lead to the development of NeuroAIDS even if HIV replication in other parts of the body is controlled through medication, Zhang said. NeuroAIDS can result in early onset dementia through damage to the brain’s synapses, which enable communication between neurons.
The significant number of opiate-addicted HIV carriers led Zhang and his peers to probe for an explanation of the link between the virus and addiction.
“This led us to ask why, from a biological standpoint, is opiate addiction related to the spread and replication of HIV in the brain,” Zhang said.
Linked receptors

The team took a step toward answering that question when it found that activation of a specific neural receptor called the μ opioid receptor (MOR) — which has a high affinity for opiates — is linked to neural HIV infection. Activation of MOR causes an increase of another receptor found in white blood cells called CCR5, which allows HIV to enter the nervous system.
“CCR5 acts as a gatekeeper. Instead of blocking HIV, it actually opens the door,” Zhang said. “The virus uses CCR5 as a way to enter the body. This receptor actually helps the virus to merge with the membrane system of cells.”
The researchers are now investigating why MOR results in an increase of CCR5. It is a discovery that would help with drug development, Zhang said. The two receptors may physically interact and cause protein actions downstream.
Zhang’s lab has developed a series of small molecules meant block the interactions between MOR and CCR5 by simultaneously affecting both targets. His team is currently testing the effectiveness of those molecules, with the hope of eventually creating therapies with the same function.
“We hypothesize that if you block MOR and CCR5 simultaneously, you will see a synergistic effect in preventing HIV viral invasion in the nervous system, and eventually treat NeuroAIDS,” Zhang said.

Mishka Terplan, M.D., a professor of obstetrics, gynecology and psychiatry at VCU School of Medicine, is proposing new approaches to how care providers treat pregnant women who are addicted to opioids.
After a systematic review of treatment practices, Terplan found that access to drug addiction treatment and the quality of these services should be improved for pregnant women. He advocates extensive care that goes beyond detoxification to the same level of screening that is standard for other diseases and the integration of addiction treatment with other types of care.
Terplan also notes the role of major gender and race disparities and discrimination in opioid addiction treatment.
Detoxification and pregnancy
Terplan said there is an overemphasis on detoxification, or medically assisted withdrawal, in current medical literature and practice. Part of this trend is a recent reconsideration of the longtime practice of continuing opiate-addicted pregnant women on pharmacotherapy to prevent withdrawal symptoms, he said.
While the discussion is well intentioned, Terplan said it ignores a major reason pregnant women are not receiving appropriate care. Frequently, addiction is treated only with detoxification and medicinal interventions, not with behavioral health methods as well.
“There's a clinical mismatch. If detoxification isn't paired with other levels of care, it doesn’t work,” he said. “You can’t treat a chronic disease with an acute intervention. It leads to relapse and that’s a concern because in pregnancy relapse is associated with overdose and the acquisition and transmission of HIV and Hepatitis C.”
Terplan said obstetricians and primary care physicians should screen for addiction in all women and this screening should be common across multiple health fields.
“The best vision would be addiction assessment and referral that is common, uniform and universal across all health care domains,” he said. “Just like primary care doctors are going to test you for cholesterol and check your blood pressure, they should assess if you are engaging in any hazardous substance use and whether you might have an addiction.”
Opioids, race, and gender
Opioid use and addiction are far more common among white women — a fact that has shaped clinical responses to the crisis, Terplan said.
“It's a complex topic,” he said. “There is a peculiar relationship between sex, gender and opioids. We are increasingly seeing an opioid epidemic with a young, white female face.”
Terplan attributes part of the disparity to sex differences in experiencing pain, and gender differences in psychological trauma. Pain associated with menstruation and other aspects of reproduction can contribute to higher prescription drug use. Women are also more likely to experience violence, rape and childhood sexual abuse, which may lead to the prescription of opioids to manage anxiety and depression.
As for racial disparities in addiction treatment, Terplan said racism in health care is a factor. White patients who present pain in emergency departments are more frequently prescribed opioids than black patients due to the preconception that these patients are more likely to abuse drugs.
Terplan also said race plays a role in the response of the public and health professionals once addiction diagnoses are made.
“Clearly there have been people of all races addicted to heroin since there has been heroin. But the public response to the opioid epidemic has been positive in many ways because it is white people who are the face of the epidemic,” Terplan said. “When it was black women and crack cocaine, we had a heavy-handed criminal justice response. Now that it is white suburban women with initially prescription opioids, and then heroin, we have a gentler response.”
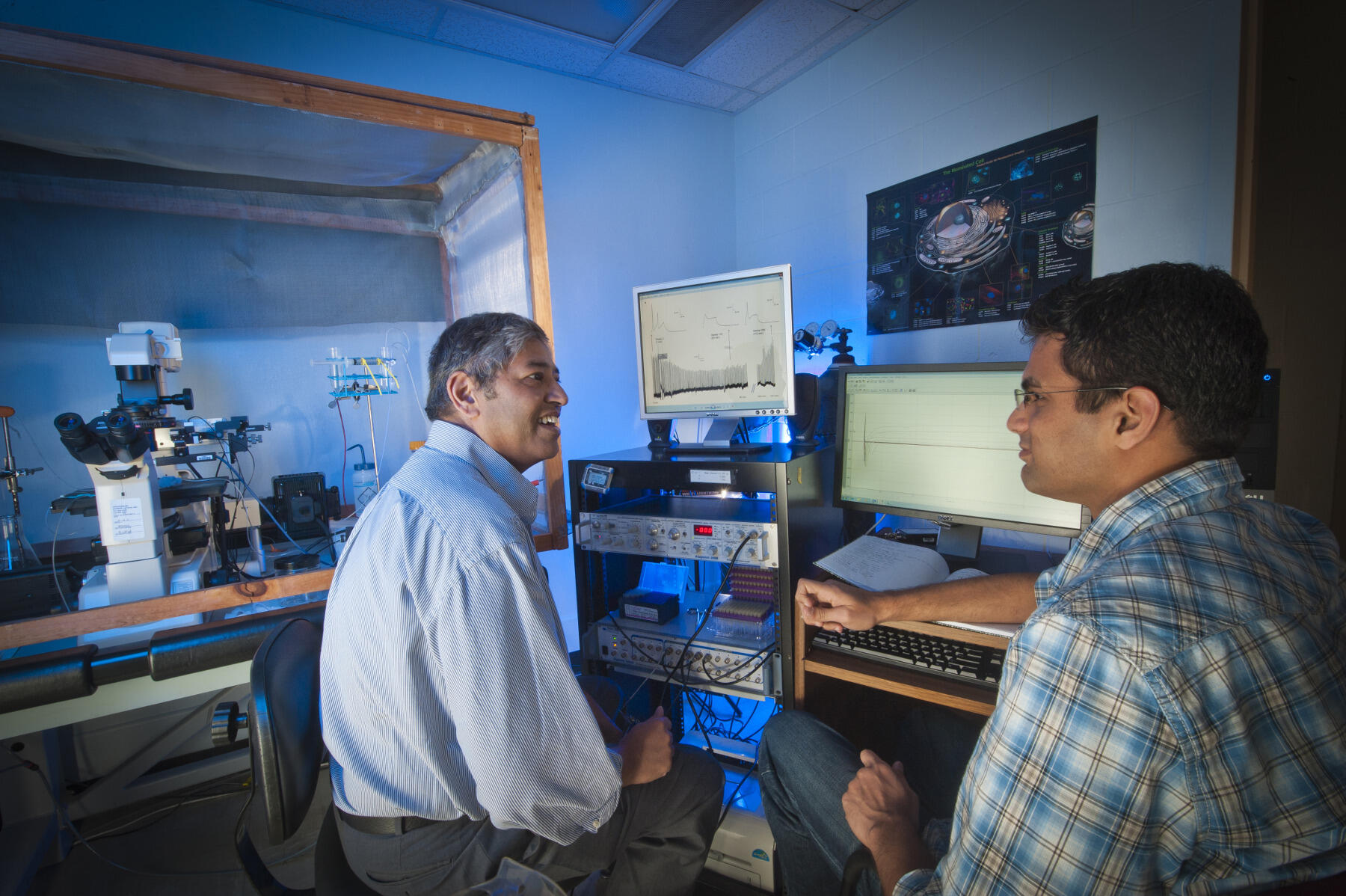
Photo by Allen Jones, University Marketing.
William Dewey, Ph.D., professor and head of the Department of Pharmacology and Toxicology in the School of Medicine; and Hamid Akbarali, Ph.D., professor and director of the department's graduate education and post-doctoral training program, have found that chronic opioid use increases the body's exposure to harmful bacteria, which contributes to addiction. The researchers are also studying the mechanisms by which opioid use causes constipation, with the goal of developing alternative drugs to prescription opioids.
Akbarali said both tolerance and opioid-related constipation are key issues to tackle in the opioid epidemic.
“Opioids are excellent analgesics, or pain killers, but it is a double-edge sword,” he said. “Tolerance develops to the pain-relieving and euphoric effects, which results in dose escalation and has led to an opioid crisis. This has also resulted in a need to treat the debilitating effects of opioid-induced constipation.”
Opioids and bacteria

Akbarali and Dewey have found opioid addiction is exacerbated by the negative effect of the drugs on the microbiome — the collection of bacteria and other microbes within the gut. Opioid use changes the microbiome by increasing the ratio of harmful bacteria to beneficial bacteria, and may allow the development of stronger, more pathogenic bacteria. It also causes the breakdown of the epithelial barrier, which protects the wall of the colon from bacteria. When the colon is compromised, an immune response produces cytokines, signaling molecules that cause inflammation.
It is a toxic chain of events with dire consequences, Akbarali said. Cytokines are particularly harmful because they cause neurons to develop greater tolerance to the pain-numbing effects of opioids. Opiate abuse then becomes more likely because chronic users become more resistant to the effects of the drugs.
Akbarali and Dewey intend to use these findings to develop alternatives to opioids that have the same analgesic capabilities without the risk of inflammation. But more must be discovered about the mechanisms that allow the gut bacterial change to increase tolerance.
“We have found that the gut bacteria itself is actually affecting the functioning of the brain,” Akbarali said. “Imagine preventing tolerance from developing so that you don't have to keep taking more. That is the benefit of finding out how the brain develops tolerance.”
Opioids and constipation
Both researchers are also working to develop pain-relief alternatives to prescription opioids that don’t cause constipation, which results from chronic opioid use.
Chronic constipation can cause a bloated colon that could eventually perforate, which results in septic shock and death.
Not only is constipation dangerous, it’s excruciatingly painful, Dewey said.
“You have people in the hospital with severe cancer pain but the discomfort of the constipation that develops from prescription opiate use is worse than the cancer pain, so they lay there and say ‘no more opiates,’” Dewey said. “That’s terrible. We should be able to figure out a solution. We as a community of researchers are smarter than that.”
Subscribe for free to the VCU News email newsletter at http://newsletter.news.vcu.edu/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Monday and Thursday during the academic year.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.