Feb. 16, 2026
How to plan for a ‘good death,’ according to a VCU researcher
Share this story
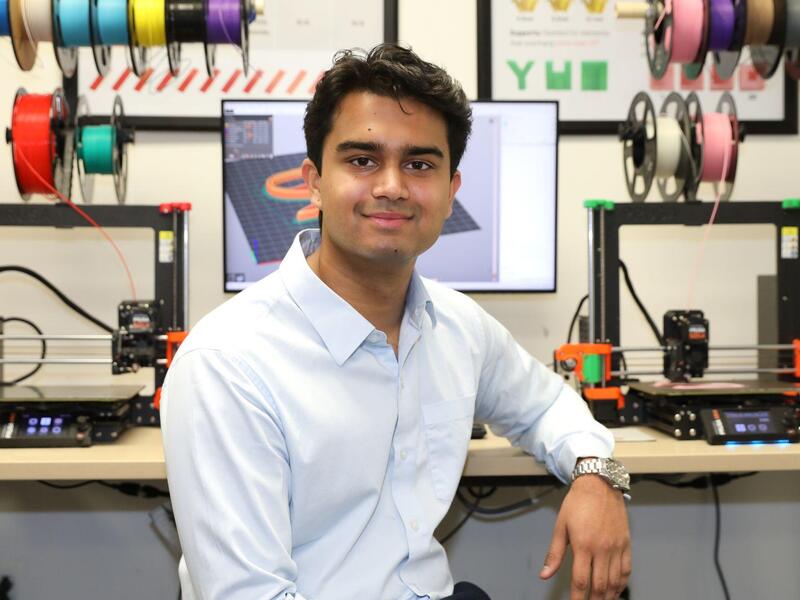
People talk a lot more about death than dying. That’s according to Yifan Lou, Ph.D., a Virginia Commonwealth University School of Social Work assistant professor who studies how expectations around death and end-of-life care differ across cultures.
“When I say ‘end-of-life care plan,’ they only think about the funeral or the moment of death,” she said.
But there’s a lot more to it than that, and that widespread misunderstanding can lead to family problems, financial confusion and patient distress, Lou said. Fortunately, social workers can step in, providing culturally sensitive care and ensuring that those nearing the end of life experience a “good death” – whatever that may look like to the patient.
“Everyone wants their good death, but it’s a really a privilege in the United States to have a good death,” Lou said. “My job is really trying to understand different populations and then help design a policy and health care system that can support their value of the good death.”
Planning for a good death requires patients and families to make decisions around hospice care, pain management, quality of life, financial affairs and long-term care, ideally alongside a social worker. But those factors are influenced by both individual preferences and cultural expectations.
“Social workers aren’t judgmental about whether patients want life-sustaining treatment or if they want hospice care,” said Lou, who worked as a hospital social worker before graduate school. “What I care about as a social worker is that they have choice and they know they have options.”
Lou recently received approximately $100,000 in funding to conduct three studies focusing on the end-of-life-care needs and perspectives of Chinese Americans and rural Americans.
VCU News spoke with Lou about her research, social work and end-of-life care across cultures.
What does a “good death” look like across different cultures?
Everyone has their own idea of what a good death looks like. People have different preferences around many aspects of death and dying – from where they want to receive care and what treatments they want to how they wish to be remembered – and these preferences are strongly shaped by culture.

For example, some older adults in Asian countries may prefer not to be fully informed about their prognosis or directly involved in decisions, choosing instead to leave these choices to their families. These preferences challenge the current person-centered care model on the ground in the United States and other Western countries, which assumes older adults should make decisions independently, without involving family members.
What factors contribute to someone having a good death?
Consistent across studies, a good death marked by better quality of life is more likely for individuals who are white with a higher socioeconomic background. But here’s the surprising part when it comes to health-related individual factors, based on my research: People who cycle through a whole range of treatments – surgery, dialysis and eventually hospice – actually tend to have a worse end-of-life experience than those who never used hospice at all.
It seems that, despite everyone’s best efforts, coordinating and trying every possible treatment can take a toll, often at the expense of quality of life in the final days. And this is precisely where social workers can play a crucial role, advocating for patients throughout the care coordination, decision-making and management process.
How would you like to see the end-of-life care system in the United States change for the better?
First, it really needs to be individualized, humanized and flexible enough to be able to honor each person’s different preferences for a good death. Second, end-of-life care doesn’t start at the very end – values and preferences are shaped long before that.
For instance, individuals who have had negative health care encounters may feel less empowered to engage in end-of-life care planning. One of my recent studies shows that how people perceive whether their wishes were respected in past health care encounters explains much of the disparity between Black and white Americans in end-of-life planning.
If we want a truly better end-of-life care system, we have to think broadly, improving not just care at the final stage of life but the health care experiences that shape people’s choices along the way.
How can we reshape how we think about the end of life and dying?
Be open. Be open to the topic of end-of-life care, recognizing that eventually, every one of us will face death.
Don’t assume that doctors you’ve seen for decades, or even your loved ones, automatically know your preferences. Be open to planning in advance. People often focus on funerals or the moment of passing, without realizing that advances in medical care mean that active dying can sometimes last months or even years, so there are a lot of medical and financial decision-making that needs to be done.
How can social workers help?
Social workers play a central role in end-of-life care. Beyond providing psychological and emotional support to patients and families, they bring unique strengths in care coordination and advocacy, ensuring that older adults’ needs, values and preferences are respected within a complex health care system.
End-of-life care is inherently collaborative, and social workers often serve as the “glue” within interdisciplinary teams. In a medically driven end-of-life care system, social workers play a distinctive role in humanizing care.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.